In the intricate landscape of the human body, a silent war is constantly being waged. Our immune systems are designed to be the ultimate sentinels, identifying and neutralizing threats with surgical precision. Yet, for decades, cancer has been the ultimate escape artist, a master of disguise that manages to hide in plain sight by mimicking our own healthy cells. The challenge for modern medicine has always been to find a way to unmask these intruders without harming the patient. Now, a breakthrough from the Department of Bio and Brain Engineering at KAIST is changing the rules of engagement. By harnessing the power of artificial intelligence, researchers have discovered a way to not only identify the unique signatures of cancer but to train the immune system to remember them forever.
The Hidden Map of the Enemy
At the heart of this discovery are neoantigens. These are tiny protein fragments, born from the chaotic mutations within a cancer cell, that act as unique biological markers. Because they exist only on cancer cells and never on healthy ones, they are the “holy grail” of personalized medicine. If a vaccine can teach the immune system to recognize these neoantigens, it can trigger a targeted strike that ignores everything else. While global giants like Moderna and BioNTech have used mRNA platforms—the same technology that powered COVID-19 vaccines—to begin exploring this frontier, the path to a perfect cancer vaccine has remained elusive.
The problem has been a matter of perspective. For years, the scientific community has focused almost exclusively on T cells, the “infantry” of the immune system that hunts and kills infected or cancerous cells directly. However, focusing only on T cells is like fighting a war with only half an army. To truly defeat an enemy as resilient as cancer, the body needs more than just a frontline attack; it needs a strategic reserve and a long-term memory. This is where the B cell comes into play.
Enlisting the Missing Half of the Army
B cells are the master architects of immunity. While T cells are famous for their direct combat roles, B cells are responsible for producing antibodies and, perhaps more importantly, establishing the long-term memory that prevents a disease from returning. Despite their critical role, they have been largely ignored in the design of cancer vaccines. As the research team points out, Professors Mark Yarchoan and Elizabeth Jaffee at Johns Hopkins University recently highlighted this gap in the scientific record. They noted that “despite accumulating evidence regarding the role of B cells in tumor immunity, most cancer vaccine clinical trials still focus only on T cell responses.”
The researchers at KAIST, led by Professor Jung Kyoon Choi and working in collaboration with Neogen Logic Co., Ltd., realized that a truly effective vaccine must be a dual-threat system. By adding B cell reactivity to the equation, cancer vaccines can move beyond one-time attacks and short-term memory to become a long-term immunity that “remembers” cancer, effectively preventing recurrence. To achieve this, they turned to artificial intelligence.
A Digital Brain for Biological Precision
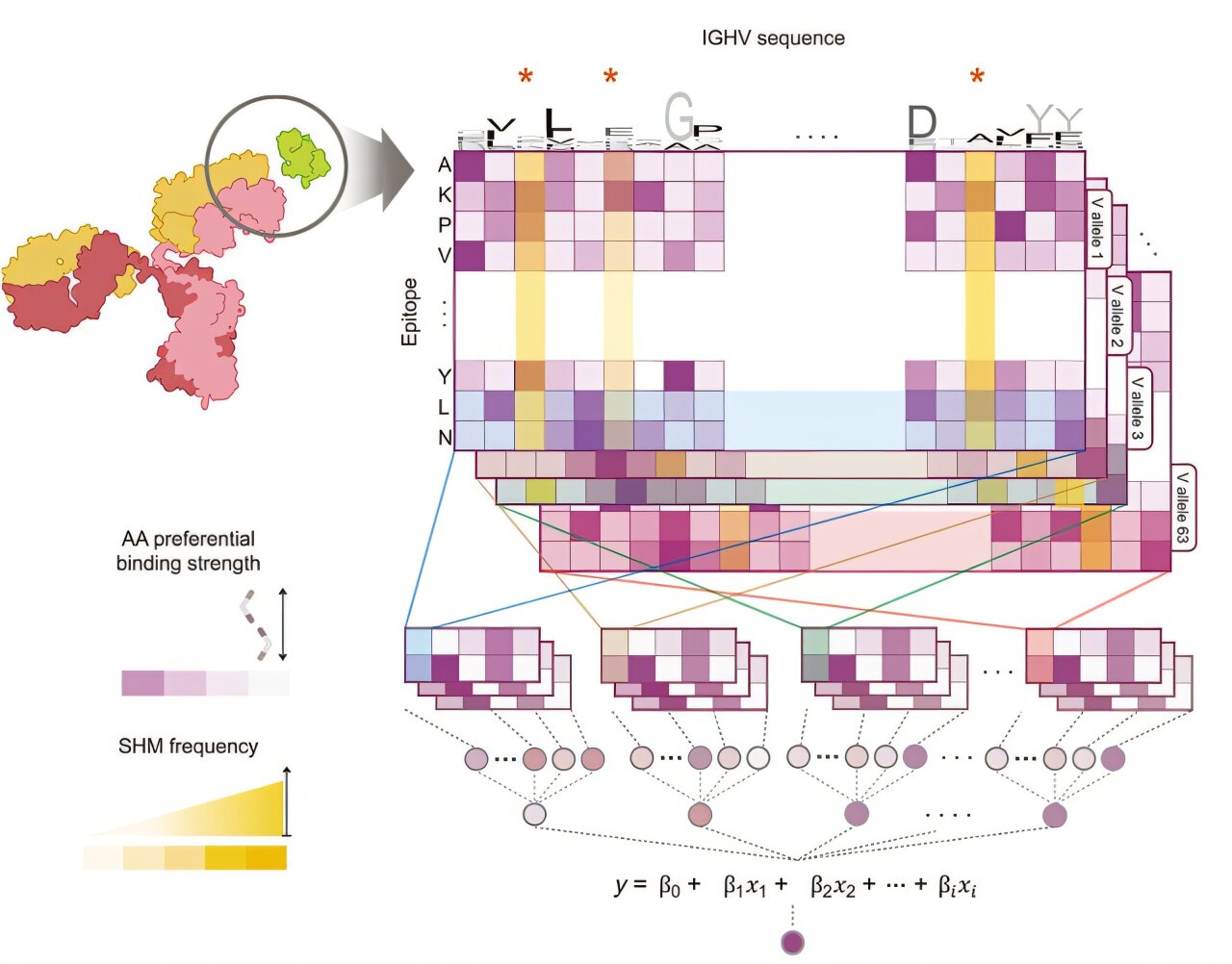
The team developed a sophisticated AI model designed to predict which neoantigens will most effectively trigger a response from both T cells and B cells. This was no simple feat. To understand how a B cell will react to a mutated protein, the AI had to learn the incredibly complex structural binding characteristics between mutant proteins and B cell receptors. It is a biological puzzle of infinite possibilities, requiring the AI to simulate how these molecules “dock” with one another in three-dimensional space.
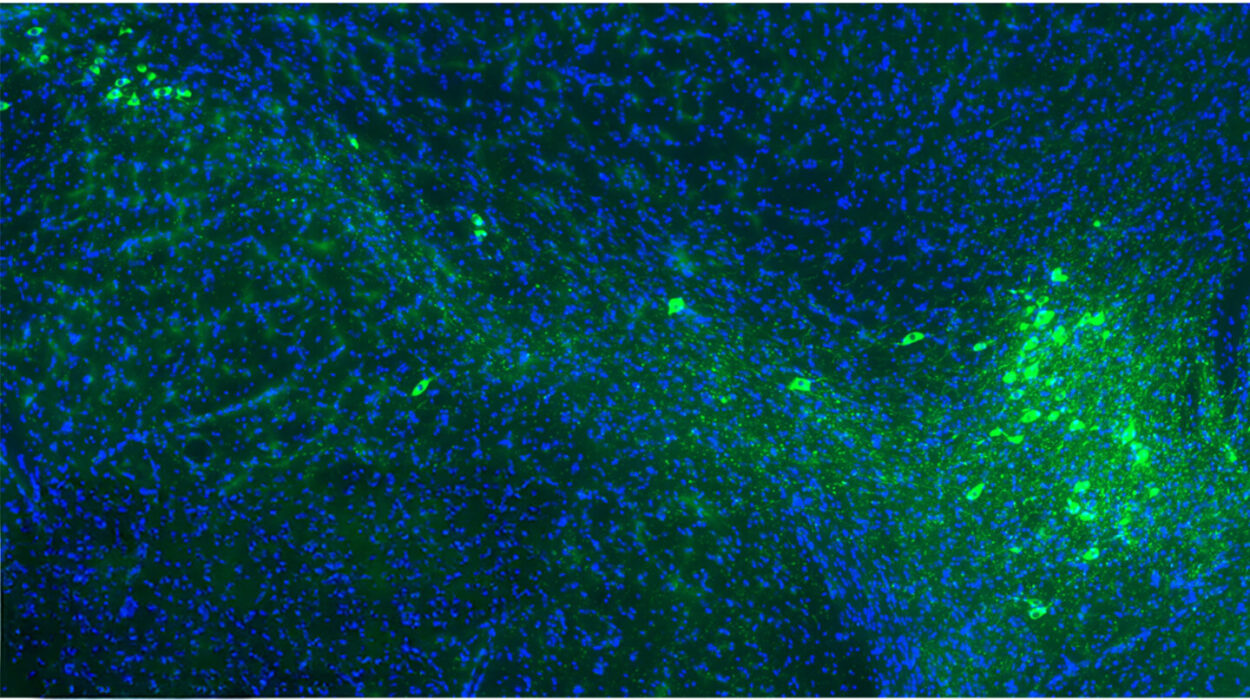
This technology represents a massive leap forward as the first AI capable of quantitatively predicting B cell reactivity to neoantigens. The researchers didn’t just stop at theoretical models; they validated their digital predictions against the real world. They ran their AI against large-scale cancer genome data, performed animal experiments, and even analyzed data from human clinical trials. The results were clear: when a vaccine is designed to stimulate both T cells and B cells, the anti-tumor immune effect is significantly enhanced. The AI provides a blueprint for a personalized vaccine tailored to the specific genetic makeup of an individual’s tumor, ensuring the most potent immune response possible.
The Dawn of Personalized Protection
The implications of this research are moving rapidly from the laboratory to the clinic. Professor Jung Kyoon Choi and his partners at Neogen Logic Co., Ltd. are currently in the midst of pre-clinical development. Their goal is ambitious but grounded in the success of their new model. They are preparing to submit an Investigational New Drug application to the FDA, with the aim of entering human clinical trials by 2027.
Professor Choi explains the vision for the future of this work: “Together with Neogen Logic Co., Ltd., which is currently commercializing neoantigen AI technology, we are conducting pre-clinical development of a personalized cancer vaccine platform and are preparing to submit an FDA IND with the goal of entering clinical trials in 2027. we will enhance the scientific completeness of cancer vaccine development based on our proprietary AI technology and push forward the transition to the clinical stage step-by-step.” This step-by-step progression is the bridge between a breakthrough in a computer lab and a life-saving treatment in a hospital.
Why This Matters for the Future of Medicine
This research matters because it addresses the single greatest fear of any cancer survivor: recurrence. Current treatments are often effective at removing the initial threat, but they frequently fail to leave the body with the tools it needs to keep the “guards” on duty. By integrating B cell reactivity into vaccine design, science is moving toward a future where a patient’s own immune system becomes a permanent, self-updating defense system.
By using AI to bridge the gap between T cell and B cell responses, we are no longer just guessing which parts of a tumor the immune system might notice. We are providing a precise, personalized map that tells the body exactly what to look for and how to remember it. This technology doesn’t just promise a better way to treat cancer; it promises a way to ensure that once the battle is won, the war is over for good. In the world of American healthcare and global medicine, this shift toward comprehensive, AI-driven personalized immunity could represent the definitive turning point in our relationship with one of humanity’s oldest and most devastating foes.
Study Details
Jeong Yeon Kim et al, B cell–reactive neoantigens boost antitumor immunity, Science Advances (2025). DOI: 10.1126/sciadv.adx8303