For a long time, the rhythm of American life was dictated by a single, invisible force. We lived by the rise and fall of dashboards, the daily tally of case numbers, and the urgent updates from public health officials. But in May 2023, the sirens went quiet. With the end of the public health emergency declaration, the national stream of case-based data that once illuminated the path of the virus effectively dried up. To many, it felt as though the storm had finally passed, leaving behind a clear sky. However, the absence of a signal does not mean the absence of a threat. While the public eye turned elsewhere, the virus continued its quiet work, circulating through communities and placing a persistent, heavy weight on the nation’s healthcare system.
The Hidden Count in a Quiet Room
When case reporting officially ended, it created a vacuum of information. Scientists at the Centers for Disease Control and Prevention (CDC) knew that they could not react to what they could not see, and yet the virus was becoming increasingly difficult to track. Mortality tracking typically relies on death certificates, but these are only as accurate as the testing and reporting that precede them. In a world of relaxed reporting requirements, new variants, and a general reduction in testing, the true toll of the virus began to slip into the shadows. Many people who feel the familiar ache and fever of a symptomatic illness no longer seek formal medical care or testing, creating vast gaps in the data regarding attributable illnesses and deaths.
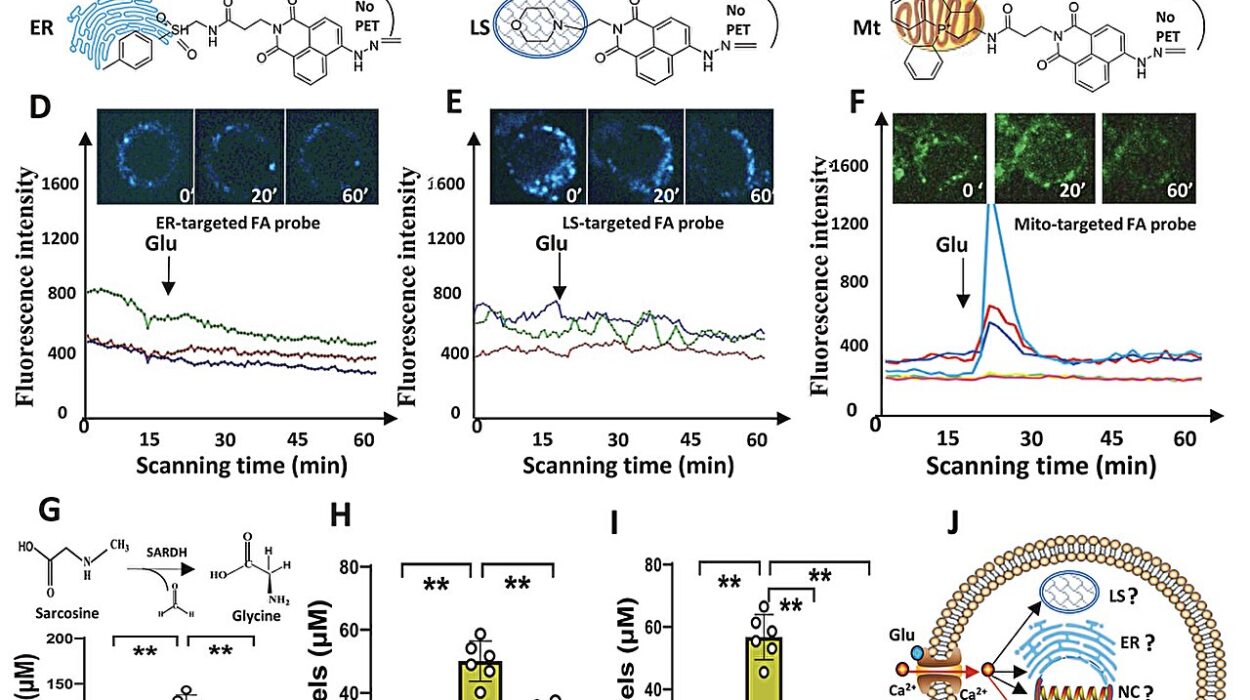
To find the truth hidden in these gaps, researchers turned to the sophisticated world of “hierarchical Bayesian modeling” and “probabilistic mathematical multiplier models.” This wasn’t just about counting heads; it was about using math to see the invisible. By taking known data points and accounting for the likelihood of underreporting and missed cases, they sought to rebuild a complete picture of the two years following the end of the emergency phase. They focused their lens on two distinct periods: October 2022 to September 2023, and October 2023 to September 2024.
Mapping the Ghost of a Pandemic
The researchers didn’t have to start from zero. They utilized the COVID-19 Hospitalization Surveillance Network, known as COVID-NET. This network acts as a scout, pulling data from 89 counties and jurisdictional equivalents across 12 states. While this only covers about 10% of the United States population, it provides a massive sample size—94,363 participants in the first year of the study and 72,176 in the second. By applying their mathematical models to this cross-section of America, the scientists were able to generate national estimates that reveal a startling reality: the virus never actually left the building.
During the first window of time, from late 2022 through late 2023, the researchers estimated there were a staggering 43.6 million COVID-19-associated illnesses. This led to 10.0 million outpatient visits and over 1.1 million hospitalizations. Most sobering of all was the estimate of 101,300 deaths. As the calendar turned to the 2023–2024 period, the numbers shifted slightly but remained formidable. The total illnesses dropped to 33.0 million, with 7.7 million outpatient visits and 879,100 hospitalizations. Yet, despite fewer total illnesses, the death toll remained almost identical, with an estimated 100,800 lives lost.
The Burden Carried by the Elders
As the story of these two years unfolded, a clear and heartbreaking pattern emerged regarding who was bearing the brunt of the virus. The data revealed a heavy “concentration of severe outcomes” among the oldest members of society. In the 2023–2024 period, adults aged 65 years and older made up only about 17.7% of the total US population. However, their footprint in the medical data was disproportionately large. This age group accounted for nearly half—47.9%—of all COVID-19-associated illnesses.
The disparity grew even more dramatic as the severity of the cases increased. Those 65 and older accounted for 64.3% of outpatient visits and 67.6% of all hospitalizations. When the researchers looked at the ultimate price paid, the statistics were stark: this demographic represented 81.2% of all deaths associated with the virus. These aren’t just numbers; they represent a generation that continues to face a level of risk that much of the younger population has largely moved past.
A Bridge Left Uncrossed
Despite the clear evidence that the virus remains a lethal threat, the researchers found a troubling disconnect between the tools available and the people using them. We have entered an era of “prevention and treatment gaps.” Vaccination and early antiviral treatments are the primary shields against the most severe consequences of the virus, yet these shields are being picked up by fewer and fewer people. By 2024, estimates showed that only 18% of all US adults had received a recent COVID-19 vaccine. Even in nursing homes, where the risk is highest, only 30% of residents were up to date.
The story of treatment followed a similar, disappointing arc. Even when people did get sick, the life-saving potential of medicine wasn’t fully realized. In 2024, outpatient antiviral treatment reached fewer than one-half of the adults aged 65 years and older who were eligible. This gap between scientific capability and actual application means that many hospitalizations and deaths that could have been prevented are still occurring, adding unnecessary pressure to a healthcare system already struggling with the return of winter respiratory illness seasons.
Why This Research Matters
This study serves as a vital wake-up call for a society that has largely decided the pandemic is a chapter in a history book rather than a current event. The primary danger highlighted by the CDC researchers is that “assumptions can begin to shape personal choices as well as national policy when a surveillance network stops reporting.” When we stop seeing the data, there is a “real danger that people will assume the risk is gone.”
The reality is that “COVID-19 hasn’t gone away,” and it continues to place a massive burden on the American healthcare system through millions of medical visits and hundreds of thousands of hospitalizations annually. By providing these estimates, the research ensures that public health policy and resource allocation are based on the actual state of the nation’s health, rather than on the hope that the virus has disappeared. Most importantly, it reminds us that “vaccines are still actively preventing severe illness and death.” For the millions of Americans, particularly the elderly, who remain in the crosshairs of this virus, the information in this study is not just data—it is a map for survival in a world where the threat is no longer televised, but is very much still present.
Study Details
Emilia H. A. Koumans et al, Estimated Burden of COVID-19 Illnesses, Medical Visits, Hospitalizations, and Deaths in the US From October 2022 to September 2024, JAMA Internal Medicine (2026). DOI: 10.1001/jamainternmed.2025.7179
David C. Grabowski, The Continuing Burden of COVID-19 on Older Adults, JAMA Internal Medicine (2026). DOI: 10.1001/jamainternmed.2025.7187