Inside the intricate architecture of the human brain, a quiet and invisible process begins long before we notice the first flicker of a forgotten name or a misplaced set of keys. For decades, the scientific community has viewed the decline of cognitive health as a late-stage tragedy, but new research is revealing that the seeds of neural change are planted much earlier in life than previously understood. At the University of Colorado Anschutz, a team of researchers has begun to peel back the layers of this biological mystery, discovering that while the loss of brain neurons may be a lifelong trajectory, we might already possess the tools to slow it down. The story of this discovery is not just one of decay, but of a decades-old drug that may have a second life as a shield for the mind.
The Invisible Clock Within Our Blood
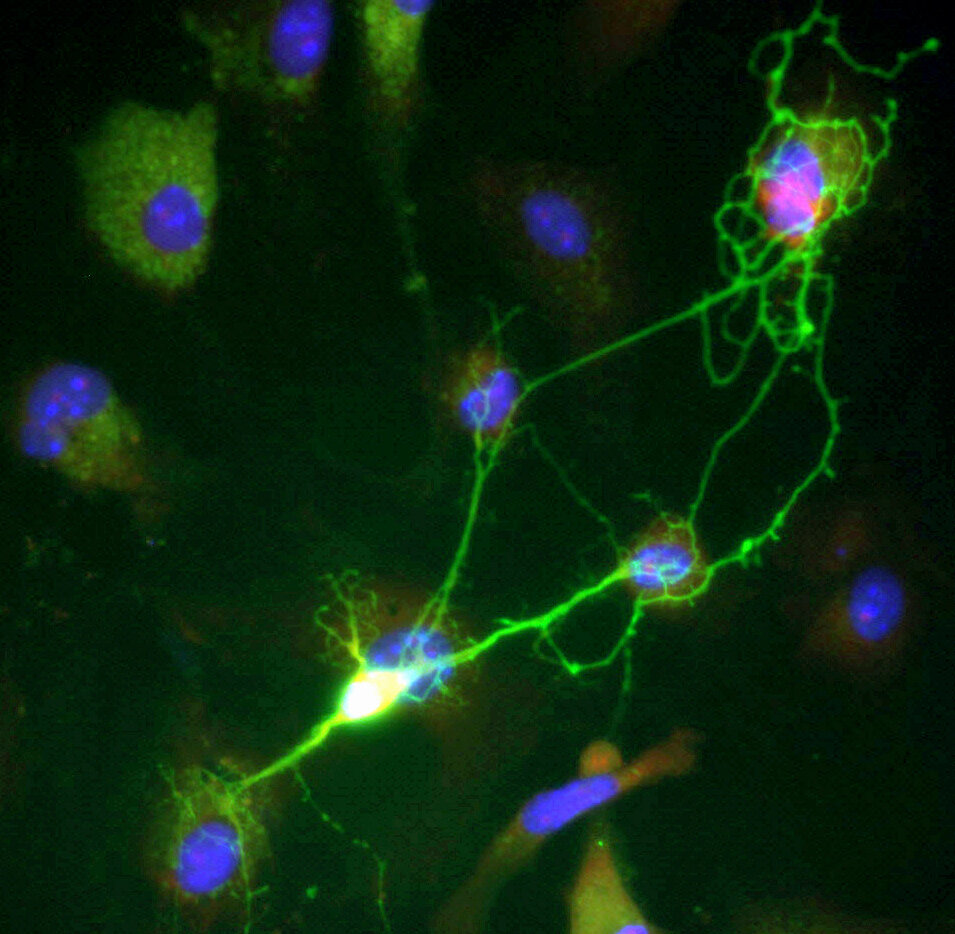
Every year we age, our bodies leave behind a molecular trail of our internal health. To understand how the brain changes over time, scientists led by Professor Huntington Potter, Ph.D., turned their attention to specific proteins that act as messengers of distress. In a cross-sectional study involving people of all ages, the researchers looked closely at a protein called UCH-L1, which is released into the blood when brain neurons die, and another called NfL, which signals that neurons have been damaged. What they found was a striking biological timeline: in early life, these proteins exist at very low concentrations, but as the years pass, their levels do not just rise—they climb exponentially.
This steady, upward march continues all the way through age 85. While these early-life changes likely reflect the normal, expected process of aging, the stakes change as we grow older. In the later stages of life, the surge of UCH-L1 in the blood becomes a harbinger of poorer outcomes, linked directly to the progression of Alzheimer’s disease and other cognitive issues. The discovery suggests that our blood carries a ticking clock of neural health, one that could eventually allow doctors to test for cognitive decline and implement therapies long before the symptoms of memory loss become irreversible.
A Gendered Divide and the Spark of Inflammation
As the researchers charted these molecular patterns, they stumbled upon an intriguing and unexplained divergence. They began monitoring a third protein, GFAP, which serves as a specialized measure of brain inflammation. Scientists believe this inflammation is a primary driver behind cognitive decline, acting as a sort of internal friction that wears down the brain’s efficiency. The data showed that GFAP levels begin to climb significantly starting at age 40, marking a turning point in the brain’s internal environment.
However, the clock seems to tick differently for men and women. The study revealed that age-associated blood concentrations of both GFAP and the neuron-death marker UCH-L1 are higher in women. The reasons for this disparity remain shrouded in mystery, yet the finding highlights a critical need to understand how gender influences the path toward Alzheimer’s. According to Professor Potter, these findings suggest that the exponentially higher levels of these markers, likely accelerated by neuroinflammation, may underlie the contribution of aging to cognitive decline and Alzheimer’s disease.
Reawakening the Body’s Natural Defenses
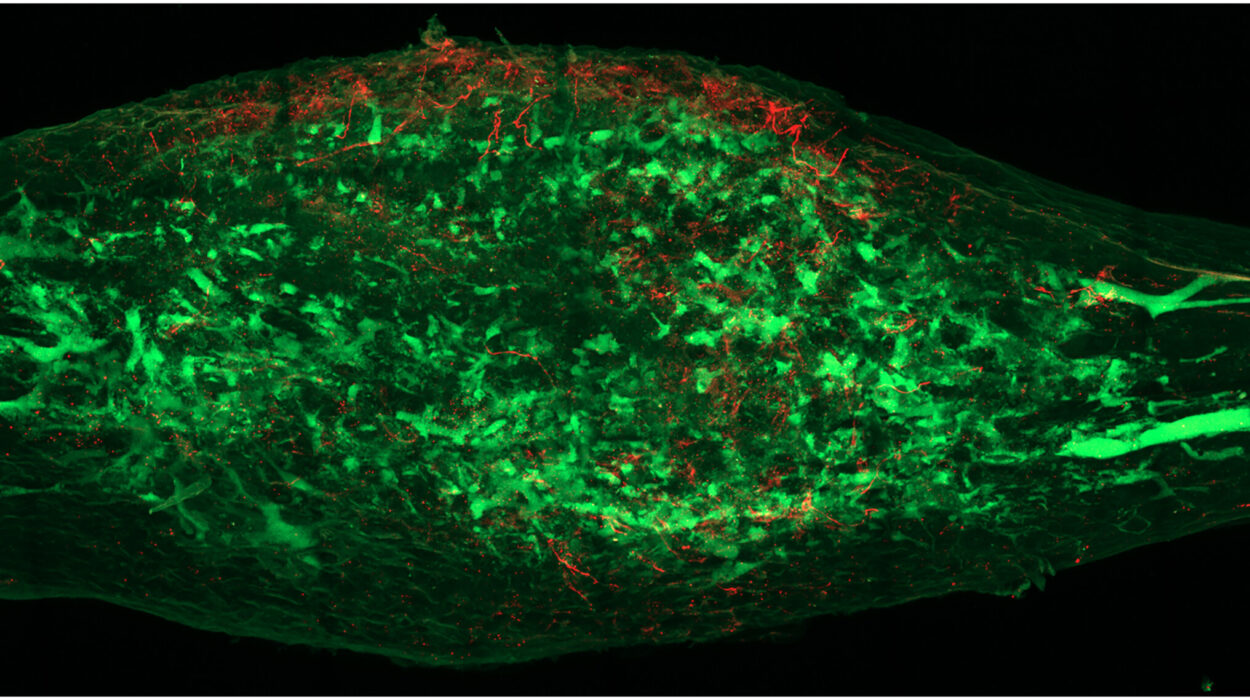
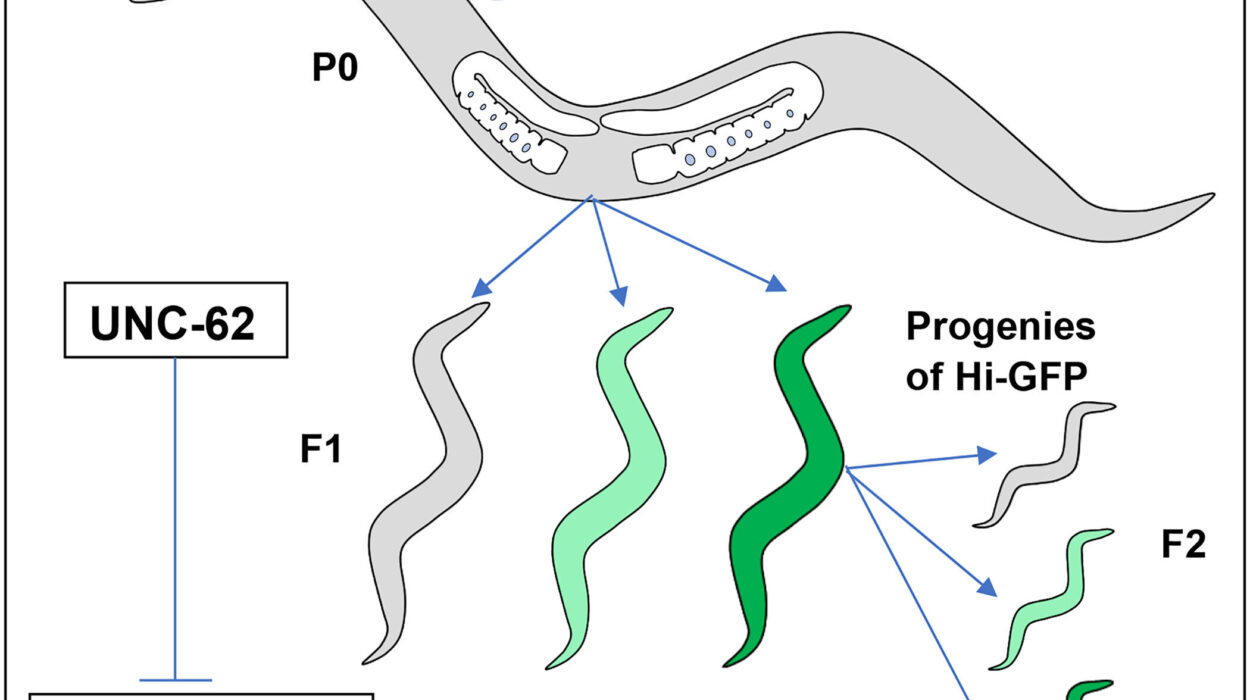
The quest to halt this trajectory led the team to a drug called sargramostim, also known as Leukine. Unlike a brand-new, experimental compound, sargramostim has been a staple in the medical world for 30 years, primarily used to treat cancer patients by stimulating their immune systems. It is a synthetic version of a natural human protein called GM-CSF, which plays a vital role in the body’s ability to heal and protect itself. In the brain and bone marrow, this protein stimulates the creation of new immune cells while simultaneously modulating inflammation.
In animal models, the results were nothing short of remarkable. Professor Potter noted that GM-CSF reverses cognitive decline and the rate of neuron death after just a few weeks of treatment. This success in the lab paved the way for a human clinical trial, where the researchers sought to see if the drug could replicate its protective effects in people living with Alzheimer’s disease. They wanted to know if a drug designed to help the body fight cancer could also be the key to helping the brain fight off the ravages of time and disease.
Turning Back the Molecular Calendar
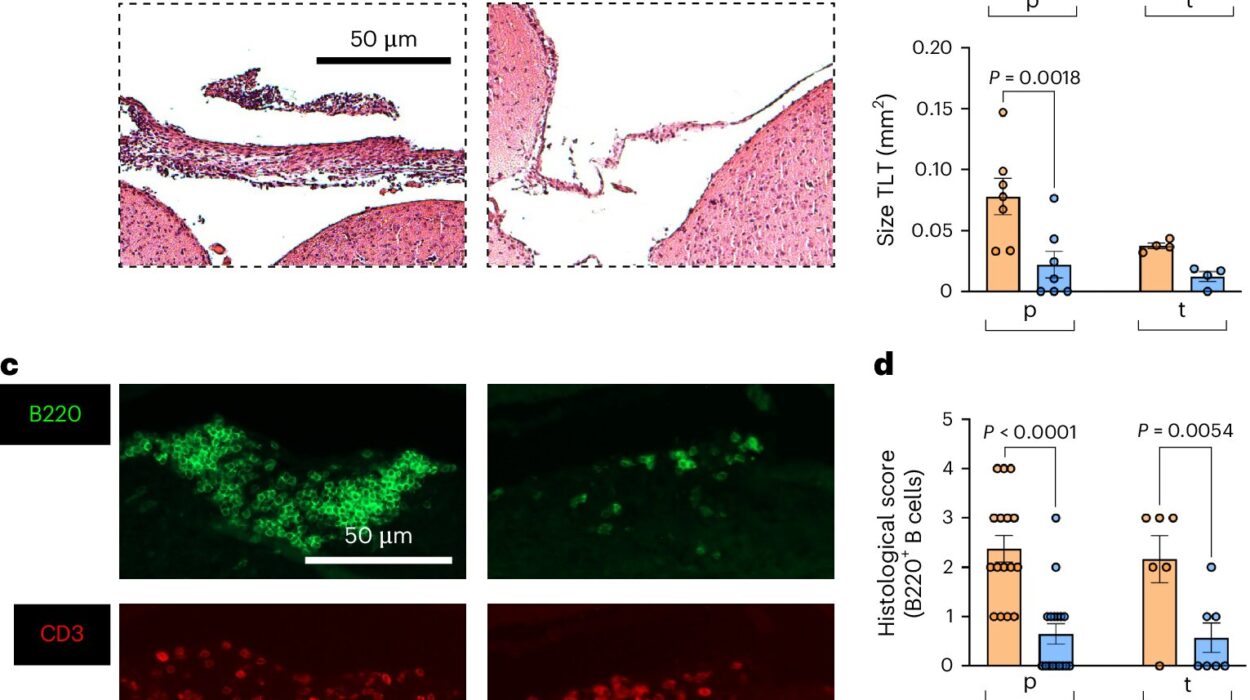
When the results of the sargramostim clinical trial came in, the data provided a startling glimpse into the drug’s potential. The participants with Alzheimer’s who received the treatment saw a dramatic shift in their internal chemistry. “When people with AD were given sargramostim in the clinical trial, their blood levels of the UCH-L1 measure of neuronal cell death dropped by 40%—in our study, this was similar to levels seen in early life,” Potter said. “We were very surprised.”
This 40% drop effectively suggested that, on a molecular level, the drug was slowing or reversing the markers of cell death to a state reminiscent of a much younger brain. Beyond the blood markers, the drug also showed an impact on how the patients functioned. Those taking sargramostim demonstrated improved scores on the Mini-Mental State Exam (MMSE), a standard test used to measure cognitive health, compared to those who were given a placebo. While other cognitive tests in the trial did not show a change, the improvement in the MMSE provided a tangible sign that the drug was doing more than just altering blood chemistry—it was reaching the mind itself.
The Persistence of Memory and the Path Ahead
One of the most fascinating aspects of the trial was how long these effects lasted. The researchers found that the improvement in blood biomarkers was tied directly to the presence of the drug; once the treatment stopped, the biomarkers of brain pathology eventually returned to their previous levels. Specifically, 45 days after the treatment ended, the concentration of UCH-L1 in the blood had climbed back to where it started. However, the story was different for the participants’ cognitive performance. Even after the drug had left their systems, the improvement in the MMSE cognitive measure was retained.
This suggests that sargramostim might trigger a lasting change in the brain’s ability to function, even if the underlying markers of damage begin to rise again. Nevertheless, many questions remain. Scientists are still working to determine if the drug requires continuous use to keep neuronal damage at bay or if it can be used to reduce the normal neuron death that comes with standard aging. Because these results are preliminary, a second, more extensive clinical trial is currently underway, focusing on participants with mild-to-moderate Alzheimer’s to provide a clearer picture of the drug’s long-term efficacy.
Why This Research Matters
This study represents a significant shift in how we approach the aging brain. By identifying that markers of neuron death and inflammation begin to rise decades before a diagnosis, researchers are opening a window for early intervention that never existed before. The discovery that sargramostim can slash a key marker of cell death by 40% offers a rare “proof of concept” that the trajectory of Alzheimer’s and cognitive decline is not inevitable.
“This drug improved one measure of cognition and reduced a blood measure of neuron death in people with AD in a relatively short period of time in its first clinical trial,” Professor Potter noted. If future trials confirm these findings, it could mean that a drug already proven safe over three decades of use could be repurposed to protect the memories and identities of millions. It offers a future where aging doesn’t have to mean the certain loss of self, providing a potential bridge between the biological realities of growing older and the hope for a clear, sharp mind throughout life. For now, the scientific community awaits further data, cautioning that sargramostim should not be used for Alzheimer’s until the FDA has fully considered the evidence and granted its approval.
Study Details
Blood measure of neuronal death is exponentially higher with age, especially in females, and halted in Alzheimer’s disease by GM-CSF treatment, Cell Reports Medicine (2025). DOI: 10.1016/j.xcrm.2025.102525 , www.cell.com/cell-reports-medi … 2666-3791(25)00598-1