Deep within the spongy interior of our bones, a silent and constant manufacturing process is underway. Every second, millions of new blood cells are forged from a specialized group of architects known as hematopoietic stem cells. These remarkable cells are the blueprints of our vitality, capable of transforming into anything the body needs, from oxygen-carrying red cells to the vigilant soldiers of the immune system. But as the years pass, this microscopic factory faces a creeping threat. Every time a cell divides, there is a risk that its DNA—the instruction manual for life—will suffer a typo. These genetic mutations accumulate as we age, and for many, they mark the beginning of a dangerous trajectory toward blood cancer.
Yet, scientists have long been puzzled by a biological mystery: why do some individuals, despite carrying these inevitable genetic errors, seem to possess an invisible shield? These people harbor the seeds of cancer within their bone marrow, but the seeds never sprout. They are resilient, standing as outliers in the face of a disease that affects the blood, bone marrow, and lymphatic system. In a landmark study published in the journal Science, a team of researchers has finally peered into the genetic code of these resilient individuals to uncover the secret of their natural defense. What they found was not a complete absence of risk, but a clever biological braking system that keeps the fires of malignancy from spreading.
The Microscopic Race for Dominance
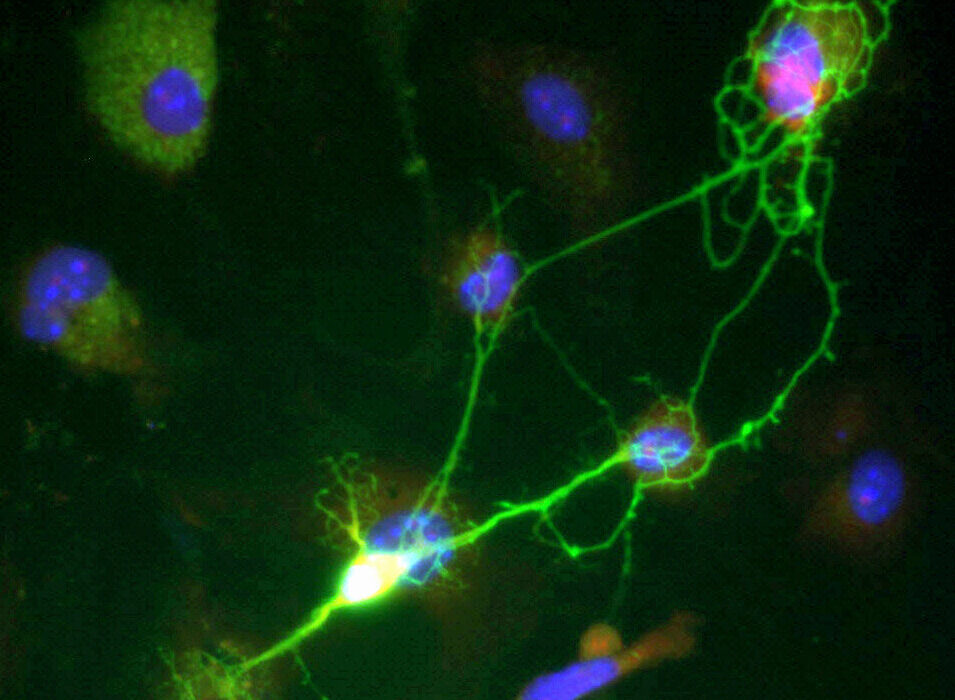
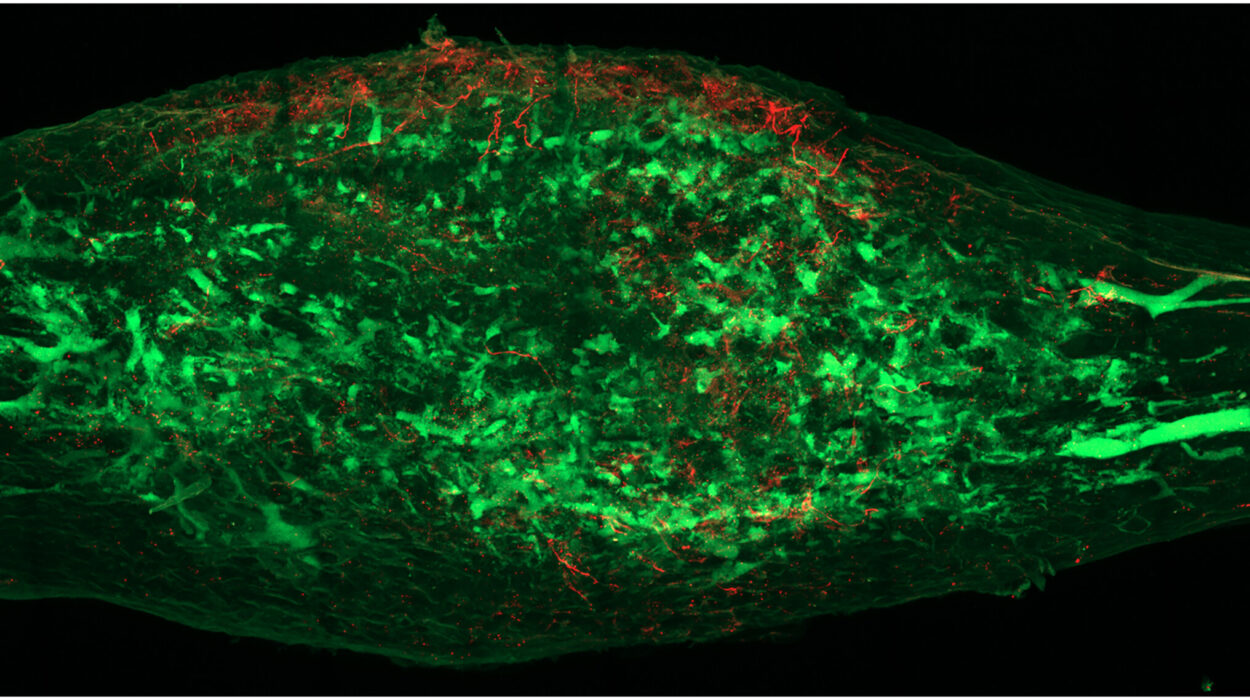
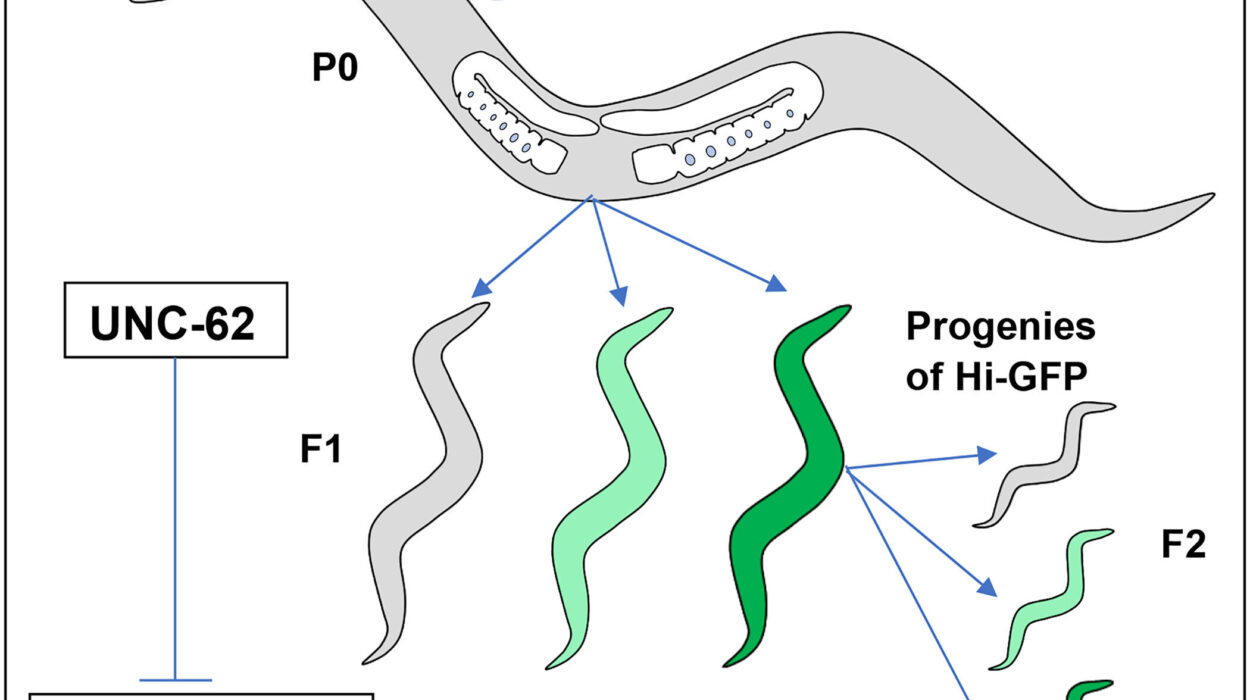
To understand this discovery, one must first look at a phenomenon known as clonal hematopoiesis, or CH. This process is essentially a race for dominance within the bone marrow. It begins when a single hematopoietic stem cell suffers a mutation that gives it a slight edge over its neighbors. Instead of functioning as a team player, this mutated cell begins to replicate itself over and over, creating a large population of identical, mutated offspring. Over time, these clones can take over the marrow, crowding out healthy cells and setting the stage for aggressive diseases like leukemia.
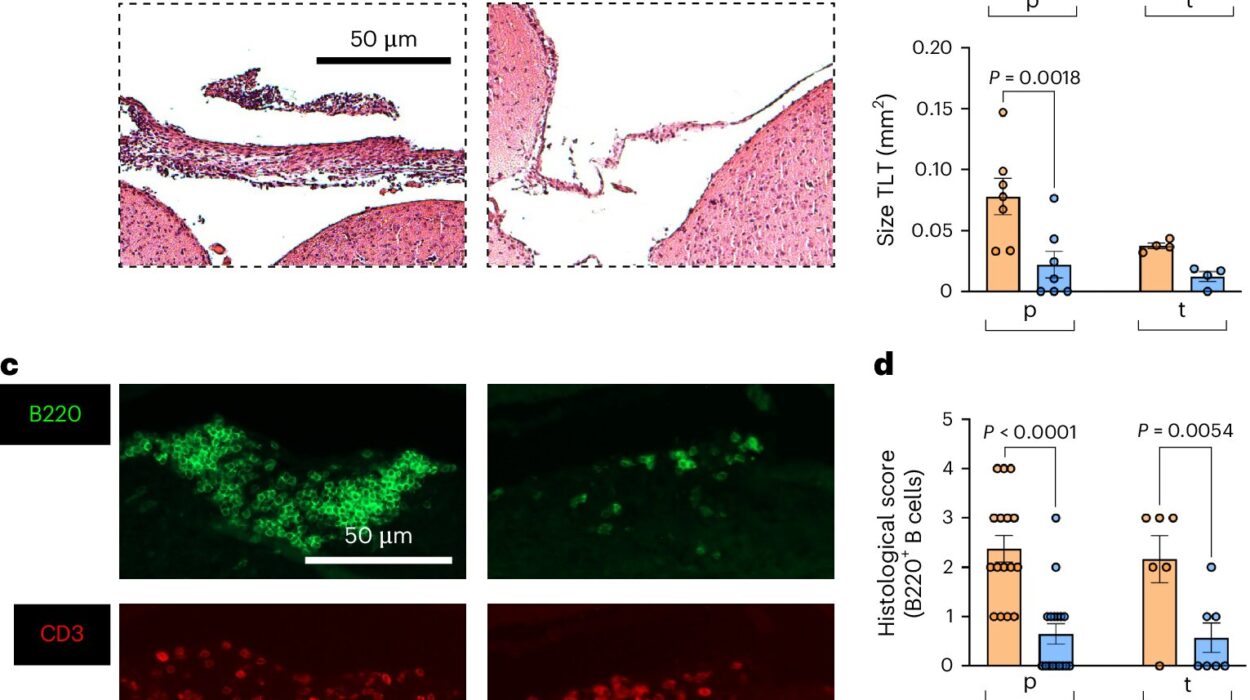
The researchers wanted to know what distinguishes the people who succumb to this process from those who manage to hold it at bay. To find out, they embarked on a massive hunt through the genetic data of more than 640,000 individuals. By conducting a large-scale analysis known as a GWAS meta-analysis, they compared 43,000 people who carried CH mutations with 600,000 who did not. They were looking for a needle in a genomic haystack—a specific genetic variant that could explain why some people’s mutated cells never grew into a dominant army.
The search led them to a quiet, often overlooked corner of our DNA. On chromosome 17q22, they identified a noncoding regulatory variant labeled rs17834140-T. Unlike many well-known genes that directly build the proteins our bodies are made of, this “noncoding” variant acts more like a dimmer switch, controlling how other genes are expressed. It was this specific switch that seemed to be the key to cancer resilience.
Taming the Growth Booster
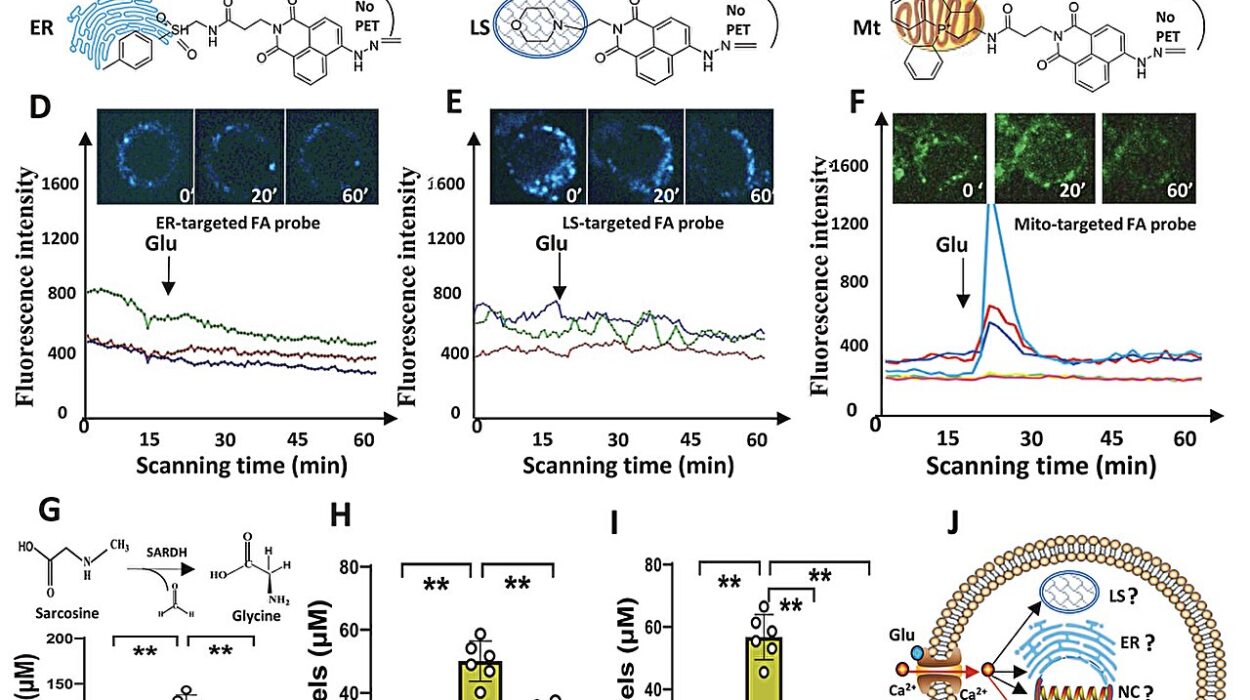
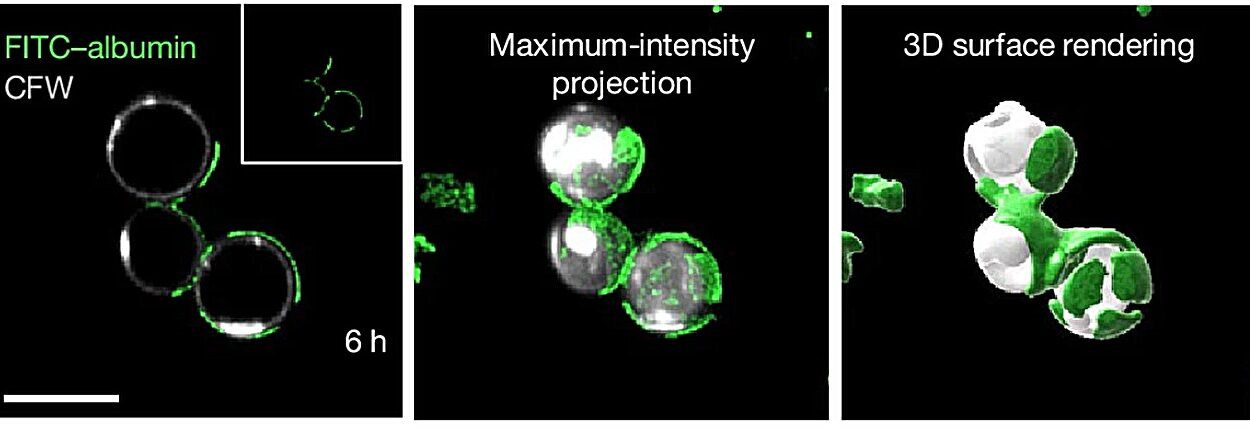
Identifying the variant was only the first step; the team needed to see it in action to understand how it actually protected the body. To do this, they turned to the cutting-edge world of lab-grown biology. Using precise gene-editing tools, they inserted the rs17834140-T variant into human stem cells. They then introduced these edited cells into mice, allowing them to observe how the cells behaved in a living environment. The results were striking and provided a clear picture of the variant’s protective power.
The secret lay in a protein called MSI2. Under normal circumstances, MSI2 acts as a potent growth booster for stem cells, ensuring they can replenish the blood supply. However, in the context of cancer, this protein becomes a liability. It fuels the rapid multiplication of mutated cells, allowing them to aggressively take over the bone marrow. The researchers discovered that people carrying the rs17834140-T variant naturally produced much lower levels of MSI2.
By lowering the volume of this growth booster, the protective variant forces mutated cells to grow much more slowly. It doesn’t necessarily delete the mutation, but it strips it of its power to expand. The study revealed that individuals with this genetic variant have up to a 30% lower risk of developing clonal hematopoiesis. In the high-stakes environment of our blood-forming system, this slow-down is the difference between a mutation that remains a harmless curiosity and one that progresses into a life-threatening leukemia.
A Blueprint for Future Defenses
The implications of this discovery extend far beyond a better understanding of our DNA. For decades, the primary strategy in oncology has been to attack cancer once it has already taken hold—a reactive approach that often involves harsh treatments. This study shifts the focus toward a new frontier: cancer prevention. By identifying the body’s own natural defense mechanisms, scientists have found a roadmap for how to stop the disease before the first symptoms even appear.
Now that the role of MSI2 is clear, the scientific community can begin looking for ways to mimic this inherited resilience in everyone. If a naturally occurring genetic variant can lower the risk of blood cancer by 30% simply by dialing down a single protein, then a drug designed to do the same could offer a powerful new tool for intervention. The researchers see a future where medical science doesn’t just treat the sick, but fortifies the healthy.
“Our study highlights the potential to target MSI2, through small-molecule inhibition or genome editing at its enhancer, for blood cancer prevention,” write the researchers in their paper. This vision of the future involves using small-molecule drugs to inhibit the protein’s activity or using genome editing to tweak the regulatory switches that control it, effectively giving a patient the same “dimmer switch” that resilient individuals are born with.
Why This Research Matters
This research marks a fundamental shift in how we perceive the relationship between our genes and disease. It moves us away from the idea that a mutation is an inevitable death sentence and toward an understanding of “resilience”—the body’s capacity to endure and overcome its own internal errors. By studying the people who don’t get sick, we are uncovering a library of biological strategies that have been refined by evolution over countless generations.
As the authors conclude, “We provide an example of how resilience to cancer can arise through inherited genetic variation, motivating the search for other natural pathways that could be leveraged to prevent or treat malignancy.” This study proves that the human body already knows how to fight back; it is now up to science to learn those lessons and apply them. Instead of merely fighting the fire of cancer, we are learning how to fireproof the building from the inside out, offering a future where the threat of blood cancer can be slowed, managed, and eventually prevented.
Study Details
Gaurav Agarwal et al, Inherited resilience to clonal hematopoiesis by modifying stem cell RNA regulation, Science (2026). DOI: 10.1126/science.adx4174
Francisco Caiado et al, Genetic resistance to leukemia, Science (2026). DOI: 10.1126/science.aed5244